Mitochondria are the power plants of cells.
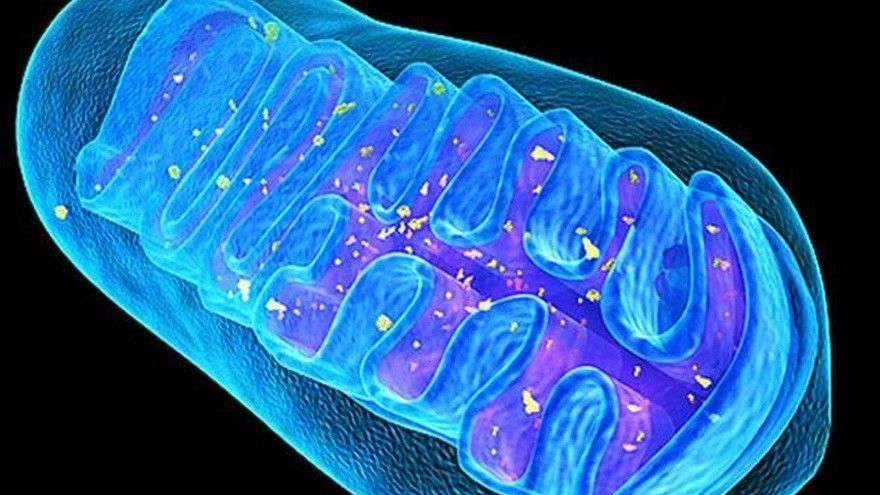
Mitochondria are the powerhouses of animal and human cells. Each tissue cell contains hundreds to thousands of mitochondria, which are organelles responsible for performing many important biochemical functions. They primarily perform many biochemical reactions in energy metabolism pathways to produce ATP, supplying more than 90% of the cell’s energy needs. An adult consumes approximately 700 kg of oxygen daily to produce 60-70 kg of ATP to maintain normal physiological activities. Simultaneously, mitochondria also participate in the biosynthesis of pyrimidine nucleotides, the regulation of intracellular calcium homeostasis, and the control of cell life and death through the translocation of apoptotic molecules.
Mitochondria are the main site of cellular production of reactive oxygen species.
During electron transport in the mitochondrial respiratory chain, reactive oxygen species (ROS) such as hydrogen peroxide (H₂O₂), superoxide anion (O₂⁻), and hydroxyl radicals (HO₂) are produced. Mitochondria are the primary site of ROS production in human and animal cells. Although some ROS and free radicals have been shown to play important roles in maintaining physiological functions, their high chemical reactivity and instability mean that excessive ROS production can damage cells and tissues through oxidation, leading to disease. The human body possesses an innate defense system to eliminate reactive oxygen species. This system primarily relies on enzymes such as CoQ10, superoxide dismutase (SOD), catalase, and glutathione peroxidase, all located within the mitochondria, for antioxidant activity.
The production of excessive reactive oxygen species induces oxidative stress.When cells
produce excessive reactive oxygen species (ROS) or when the antioxidant enzyme system is imbalanced or depleted due to aging, ROS cannot be effectively cleared, inducing oxidative stress and triggering a chain reaction of lipid peroxidation. Biochemical molecules such as DNA in the cell membrane and nucleus, and especially mitochondrial DNA, are attacked by ROS and undergo gene mutations. When mitochondrial DNA mutations reach a certain proportion, it leads to defects in mitochondrial energy metabolism. Numerous studies over the past decade have shown a close relationship between functional abnormalities caused by mitochondrial DNA mutations and the occurrence of mitochondrial diseases, age-related diseases, and metabolic syndromes.
The accumulation of oxidative damage leads to aging and degenerative diseases.
The accumulation of reactive oxygen species (ROS) leads to protein oxidative damage, metabolic abnormalities, and apoptosis. Oxidative stress-induced mitochondrial DNA mutations and lipid peroxidation are considered major causes of cellular dysfunction and aging. In the early 1990s, our laboratory was the first to report that during the aging process, mitochondrial DNA mutations accumulate, causing a gradual decline in mitochondrial respiratory function and the accumulation of ROS. Long-term research has also confirmed a close relationship between ROS and various age-related diseases such as neurodegenerative diseases, cancer, cardiovascular diseases, rheumatoid arthritis, and diabetes. Many studies have confirmed that oxidative damage causing protein denaturation and aggregation is a significant pathogenic factor in neurodegenerative diseases such as Parkinson’s disease and Alzheimer’s disease. Therefore, obtaining sufficient and diverse antioxidants from vegetables, fruits, and other foods to maintain normal mitochondrial function and enhance the antioxidant defense system within tissue cells, thereby reducing biochemical oxidative damage, is an effective strategy for maintaining health, preventing disease, and delaying aging.
Applications of human stem cells in disease treatment
For some neurodegenerative diseases, in addition to drug and surgical treatments, regenerative medicine, with stem cell transplantation as its core technology, is receiving increasing attention. The medical community hopes to use this to break through medical bottlenecks and solve diseases that are currently incurable or difficult to cure clinically. Stem cell therapy has a wide range of applications, including leukemia, diabetes, neurodegenerative diseases, and the repair of damaged tissues and organs, as well as the treatment of immune system diseases, cardiovascular diseases, and metabolic diseases. Mesenchymal stem cells have become the mainstream in stem cell therapy research and development in recent years due to their lack of ethical controversy, ease of acquisition from tissues, multi-lineage differentiation capacity, and low immune rejection. Some foreign research teams have successfully treated stroke using stem cell transplantation technology, restoring mobility to paralyzed and disabled patients. Other research teams have used neural stem cells to treat traumatic brain injury and neurodegenerative diseases. Human umbilical cord blood stem cells have been shown to produce large quantities of functional pancreatic islet cells, and their implantation into living organisms has successfully treated diabetes in mice. These major breakthroughs in regenerative medicine offer opportunities for treating diseases prevalent in modern humans. Although many stem cell studies have entered the clinical trial stage, the scientific basis for stem cell therapy is still not mature enough. The number of stem cells obtained from tissues is very small, and whether they can be successfully transplanted, differentiated, and whether they have function after differentiation are the main problems currently facing the use of mesenchymal stem cells to treat diseases.
Mitochondria and the antioxidant system play important roles in stem cell differentiation.
Over the past decade, numerous studies have revealed the crucial role of increased mitochondrial number and functional activation in human stem cell differentiation. Our research team first reported in 1998 that mesenchymal stem cells require increased mitochondrial proliferation and respiratory function during early differentiation to provide the necessary ATP. Simultaneously, the gene expression of antioxidant enzymes such as superoxide dismutase (SOD), catalase, and glutathione peroxidase also rapidly increases. Furthermore, we have demonstrated that mitochondrial dysfunction reduces the ability of human mesenchymal stem cells to differentiate into adipocytes and osteoblasts, affecting the metabolism and blood glucose regulation of differentiated adipocytes, and even inducing insulin resistance. When using autologous stem cell transplantation, the patient’s own stem cells may contain potential pathogenic factors, especially stem cells from patients with metabolic or degenerative diseases involving mitochondrial abnormalities. These patients must undergo mitochondrial function testing before clinical application. Previous studies have found that induced pluripotent stem cells derived from somatic cells in patients with mitochondrial diseases have a lower ability to differentiate into cardiomyocytes than normal individuals, indicating that normal mitochondrial function is a prerequisite for successful stem cell differentiation. Therefore, increasing the function of mitochondria in stem cells from patients will contribute to the clinical application of stem cells.
In conclusion
Biochemical and cell biological research over the past half-century has elucidated the multifaceted and important biochemical functions of mitochondria in human and animal cells. These organelles not only have the traditional function of producing ATP through energy metabolism, but also play a crucial arbitrator role in cell life and death by translocating intracellularly and extracellularly through apoptotic molecules. When tissue cells are under oxidative stress, these apoptotic molecules easily translocate to the extracellular space through mitochondrial permeability transition pores (MPTPs) on the mitochondrial membrane, initiating the cell death process. Therefore, maintaining and enhancing normal mitochondrial function and reducing (or accelerating) the production and clearance of reactive oxygen species (ROS) can prevent MPTP activation and inhibit the leakage of apoptotic proteins from the mitochondria, which should effectively reduce the occurrence of neurodegenerative diseases and age-related diseases. On the other hand, after more than a decade of research, the acquisition and large-scale culture of mesenchymal stem cells have become quite easy, and there has been rapid progress in the treatment of some diseases. However, before conducting stem cell therapy, quality control must still be ensured. The increase in mitochondrial and antioxidant enzyme gene expression during stem cell differentiation can be used as an indicator for quality assessment to improve the effectiveness and success rate of stem cell therapy.
Learn more about mitochondrial regeneration

