Stem cell exosome nebulization is a new treatment method that aims to use the bioactive substances carried in stem cell exosomes to directly act on the lesionized areas of the respiratory tract (including the nose, pharynx, throat and lower respiratory tract of the upper respiratory tract, trachea, bronchi and their branches in the lungs) through nebulization inhalation, exerting anti-inflammatory, anti-apoptotic, antibacterial and other effects to promote respiratory repair.
In autumn and winter, many people are “targeted” by respiratory diseases and cough non-stop. Some people will choose to do nebulization therapy.
At present, nebulized inhalation drugs include bronchodilators, inhaled glucocorticoids, expectorants, etc., which will have certain side effects. For example, albuterol can cause tachycardia, headache, limb tremors, etc.; ipratropium bromide can cause headache, nausea, dry mouth, difficulty urinating, etc. The earlier traditional “call triple” (dexamethasone + chymotrypsin + gentamicin) was also eliminated due to side effects.

Exosomes are nanovesicles secreted by living cells, which are responsible for cell-to-cell communication and intercellular material delivery. It has a diameter of 30-150nm and contains bioactive substances such as proteins, lipids, nucleic acids, etc., which come from their mother cells and regulate and change the function of the target cells after being absorbed by the target cells, mediating various physiological and pathological processes.
Stem cell exosomes contain bioactive substances such as growth factors and mRNA that are similar to stem cells, such as:
- Soluble growth factor (repairs damaged cells, promotes alveolar epithelial cell growth, and is involved in the growth, development and repair of lung tissue)
- Anti-inflammatory cytokines (inhibition of lymphocyte differentiation, proliferation, and production, inhibition of eosinophil proliferation and activation, inhibition of secretion of inflammatory cytokines, and mucus production of airway epithelium)
- Immunomodulators (inhibit inflammatory responses, antibacterial, bacteriostatic peptides and other cellular components directly kill local bacteria in lung tissue)
At the same time, stem cell exosomes also have the advantages of low immunogenicity, high safety and efficacy. Through nebulized inhalation, stem cell exosomes can directly reach the lesion area of the respiratory tract, reduce the distribution of drugs throughout the body, increase the concentration of drugs in the lesion area, and have the advantages of small drug dosage, large absorption surface area, rapid onset, avoidance of liver first-pass effect, and convenience of use.
Case: Stem cell exosome nebulization for the treatment of pneumonia is safe and feasible
The project “Key Technology Research on the Nebulization of Mesenchymal Stem Cell Exosomes for the Treatment of Novel Coronavirus Pneumonia (COVID-19)” (ChiCTR2000030261), which was registered in the China Clinical Trials Registry, aims to use the inhibition of inflammatory factors and enhance the body’s immunity of stem cell exosomes to promote the early recovery of patients with new coronavirus pneumonia and reduce complications by nebulizing the lungs and directly contacting the lesion. The clinical trial results of this project were published in the journal Stem Cell Reviews and Reports in 2022 (2022 impact factor 6.692).
The researchers conducted an exosome nebulization treatment trial of umbilical cord mesenchymal stem cells (MSCs) in 7 patients with new coronary pneumonia (2 severe and 5 mild). The results showed that stem cell-derived exosome nebulization therapy was safe and feasible, and MSC exosome nebulization therapy could promote the resorption of lung lesions and shorten the hospital stay of patients with mild coronary pneumonia. In addition to this, exosome nebulization therapy early in infection may be more beneficial for patients.
Mild patients recover faster after exosome nebulization therapy:
On April 3, 2020, the first CT scan of a mild patient showed that there was an isolated nodule outside the lower lobe of the left lung, on April 4, the patient received exosome nebulization therapy, on April 10, the second CT examination showed that the density of the nodules in the lower lobe of the left lung was significantly reduced, and the size was also reduced, and on April 21, the third CT examination, the left lower lung lesion was completely absorbed, and the time from the discovery of the nodule to the complete absorption of the lung lesion was 18 days。
In contrast, another mild patient with conventional treatment without nebulization had an absorption time of 27 days for lung-like lesions.
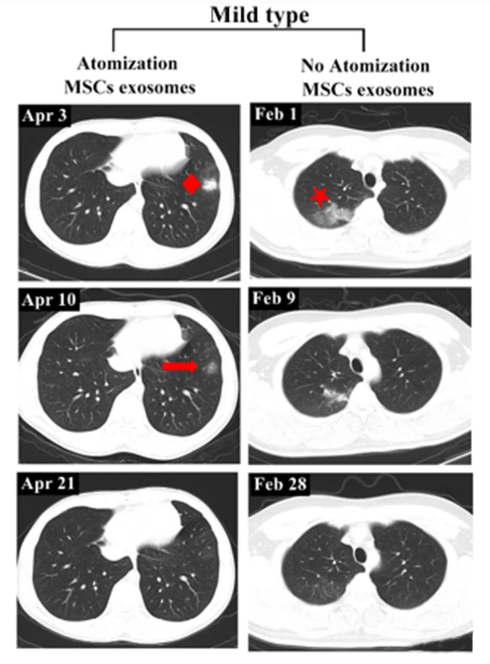
▲Left: Mild cases with exosome nebulization therapy. Right: Mild cases without exosome nebulization therapy
Severe patients recover better after exosome nebulization therapy:
A critically ill patient began exosome nebulization therapy on February 27, 2020, and on March 18, the patient’s CT scan showed significant resorption of both lung lesions and regression of lesion density. On April 1, the patient’s lung lesions were completely absorbed.
In another critically ill patient who did not receive exosome nebulization therapy, fibrous umbilical cord shadow still existed after resorption of lung lesions.
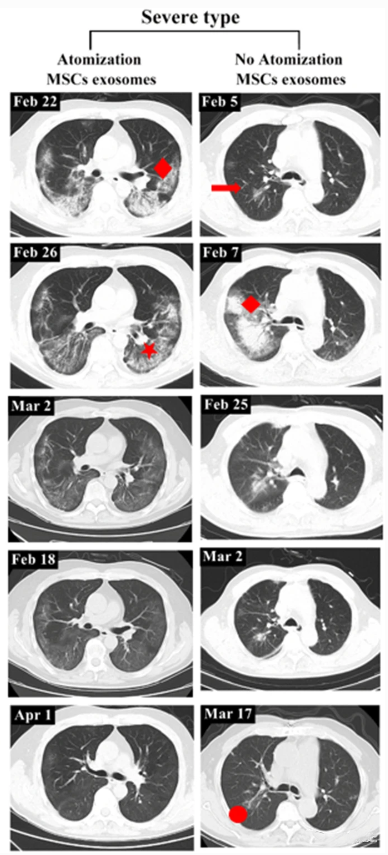
▲Left: Severe cases with exosome nebulization therapy. Right: Severe cases without exosome nebulization therapy
The sooner you use exosome nebulization, the better the effect:
CT images of the other five patients, shown below, show a significant difference between the time it takes for lung lesions to be fully absorbed after a period of antiviral therapy (patients 1, 3, 4) and those who received exosome nebulization therapy from the beginning, and those who received exosome nebulization at the beginning recovered faster.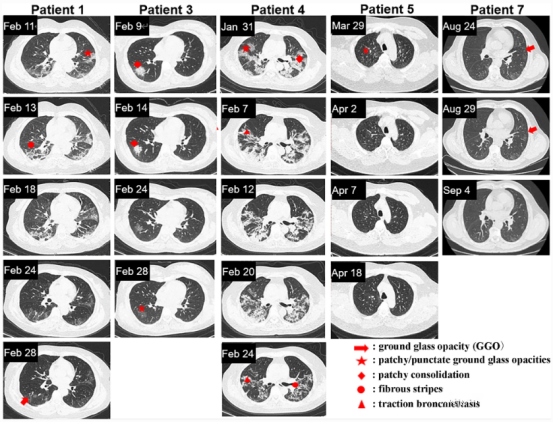
▲The recovery time of patients without exosome nebulization therapy is close to one month for 1, 3, and 4; Patients with exosome nebulization therapy had a recovery time of only about two weeks for 5 and 7.
The results of the entire clinical study show that nebulized stem cell exosomes can reach fine structures in the lungs, such as bronchioles and alveoli, to directly deliver anti-inflammatory molecules to their targets, without inducing acute allergic reactions or secondary allergic reactions, while effectively promoting the absorption of lung lesions and reducing the recovery time of patients.
Learn more about exosomes

